Trying to help someone with mental health issues only when they show signs of self-harm isn’t proactive — it’s reactive.
Counsellor Nathaniel Jewitt equates this problem to a focus on preventing suicide —but only when a person is at the edge of a cliff.
“If somebody is starting to acknowledge that they’re suicidal, there’s already been a lot of pain and suffering and that’s been going on for a while,” said Jewitt, counsellor for Carleton’s Health and Counselling Services.
More has to be done for those facing mental health issues before they reach a point where self-harm and suicide is a thought, said Jewitt, who is one of three counsellors specifically allocated to Carleton’s residences.
“Counselling isn’t the only solution for all of that. It’s how we build communities, how we teach people to make decisions and coach themselves and others through their lives,” he said.

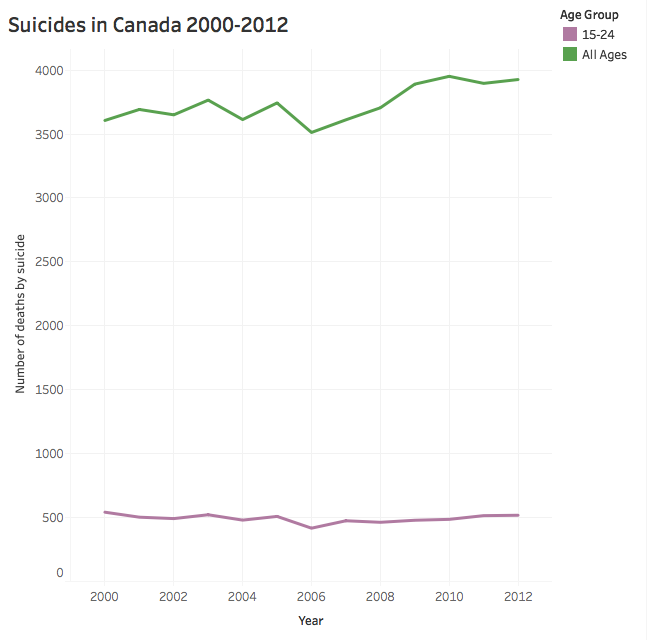
While services like counselling and crisis hotlines work to prevent suicide, the suicide rate in Canada has remained relatively stagnant since 2000 with suicides making up about 1.5 per cent of all deaths, according to data from the 2012 Canadian Community Health Survey compiled by Statistics Canada.
The above data was compiled via the 2012 Canadian Community Health Survey published by Statistics Canada. Click here to view the graph in full.
For those aged 15 to 24 the average is similar and has also remained fairly stagnant.
For Ottawans in that demographic, the average rate between 2005 and 2009 was six per 100,000 for men and four for women, according to Ontario Mortality Data extracted by the City of Ottawa.
According to Ottawa Public Health Data, about 600 women per 100,000 aged 15 to 24 were admitted to emergency rooms for self harm in 2012, with the rate being about 195 for men.
As a counsellor for students in residence specifically, Jewitt’s office is in Renfrew House on the first floor. Posters in the offices advertise for Tuesday afternoon therapy dog visits and it’s not far from where students live on the floor above. He’s one of three counsellors allocated for that office.
He said common issues among students include depression and anxiety, often related to being away from home for the first time or navigating new social environments.
Interacting with others and reminding each other that it’s normal to be imperfect tends to reduce anxiety, he said.
He said the key to preventing someone from reaching a crisis point with their mental health is to first reduce stigma surrounding valuing emotional well-being.
“It’s about taking emotional needs seriously, but also learning how to manage expectations and deal with hard times,” he said.
The above graphic was compiled using data from the 2012 Canadian Community Health Survey published by Statistics Canada and The State of Ottawa’s Health 2014 report published by the City of Ottawa.
Finding resources to help develop those abilities and navigate challenging environments can be difficult-especially for youth, said Charissa Feres.
Feres is an undergraduate student at Carleton University and Vice-President of Student Issues at the Student Alliance for Mental Health (SAMH).
Dealing with her own experiences with mental illness and trouble accessing services caused her to get involved with SAMH to help others going through similar concerns.
Recognizing that a discussion can be had about self-harm without rushing to call 9-1-1 is important, she said.
“There’s different levels to suicidality. A large amount of people who are suicidal aren’t necessarily at that level of intent,” she said.

Spaces where there isn’t fear of being sent to an emergency room are important —unless there is an imminent threat to that person’s life, and then 9-1-1 is necessary, she said.
Recognizing the core reasons for someone reaching a stage where self-harm is considered is crucial, she added.
There can be issues of secure housing, financial instability and multiple oppressions and discrimination that cannot be ignored.
“It’s not always about restricted means,” she said.
“When we talk about suicide prevention, often we are talking too late in the spectrum. We need to talk about preventing suicidal thoughts to begin with.”
Scroll over photos for captions.